WHO: Community management of opioid overdose
Death following opioid overdose is preventable if the person receives basic life support and the timely administration of the opioid antagonist naloxone. WHO recommends that naloxone be made available to people likely to witness an opioid overdose, as well as training in the management of opioid overdose.
6 Nov 2014An estimated 69 000 people die each year from opioid overdose. Opioid overdose is easily reversed with the opioid antidote naloxone and with basic life support. Such care is generally only available in medical settings, however. In 2012, the United Nations Economic and Social Council (ECOSOC) called upon the World Health Organization (WHO), in collaboration with the United Nations Office on Drugs and Crime (UNODC) to provide advice and guidance, based on scientific evidence, on preventing mortality from drug overdose, in particular opioid overdose.
These guidelines recommend that people who are likely to witness an opioid overdose, including people who use opioids, and their family and friends should be given access to naloxone and training in its use so that they can respond to opioid overdose in an emergency if a medical response is not available. Naloxone can be injected or administered intra-nasally and has minimal effects in people who have not used opioids. While naloxone administered by bystanders is a potentially life-saving emergency interim response to opioid overdose, it should not be seen as a replacement for comprehensive medical care.
Read here the World Health Organisation Community management of opioid overdose guidelines!

Key facts:
- Opioids are psychoactive substances derived from the opium poppy, or their synthetic analogues. Examples are morphine and heroin.
- Worldwide, an estimated 69 000 people die from opioid overdose each year.
- There are an estimated 15 million people who suffer from opioid dependence (i.e. an addiction to opioids). The majority of people dependent on opioids use illicitly cultivated and manufactured heroin, but an increasing proportion use prescription opioids.
- There are effective treatments for opioid dependence yet only 10% of people who need such treatment are receiving it.
- Due to their pharmacological effects, opioids in high doses can cause respiratory depression and death.
- The inexpensive medication naloxone can completely reverse the effects of opioid overdose and prevent deaths due to opioid overdose.
Opioids
Opioids are substances derived from the opium poppy, or synthetic analogues with similar effects. Examples are morphine, heroin, tramadol, oxycodone and methadone. Opioids have the potential to cause substance dependence that is characterized by a strong desire to take opioids, impaired control over opioid use, persistent opioid use despite harmful consequences, a higher priority given to opioid use than to other activities and obligations, increased tolerance, and a physical withdrawal reaction when opioids are discontinued. Dependence on prescription opioids includes iatrogenic dependence following the treatment of chronic pain, and dependence following the diversion and theft of prescription opioids from patients, medical facilities, pharmacies and the manufacturing and distrubution chains.

Opioid overdose
Due to their effect on the part of the brain which regulates breathing, opioids in high doses can cause respiratory depression and death. An opioid overdose can be identified by a combination of three signs and symptoms referred to as the “opioid overdose triad”. The symptoms of the triad are:
- pinpoint pupils
- unconsciousness
- respiratory depression.
Combining opioids with alcohol and sedative medication increases the risk of respiratory depression and death, and combinations of opioids, alcohol and sedatives are often present in fatal drug overdoses.
Because of their capacity to cause respiratory depression, opioids are responsible for a high proportion of fatal drug overdoses around the world. The number of opioid overdoses has increased in recent years, in part due to the increased use of opioids in the management of chronic non-cancer pain1. In the United States of America alone in 2010, there were an estimated 16 651 deaths due to overdose on prescription opioids and 3036 due to overdose on heroin.
Risk factors for opioid overdose
People dependent on opioids are the group most likely to suffer an overdose. The incidence of fatal opioid overdose among opioid-dependent individuals is estimated at 0.65% per year. Non-fatal overdoses are several times more common than fatal opioid overdoses.
People at higher risk of opioid overdose
- people with opioid dependence, in particular following reduced tolerance (following detoxification, release from incarceration, cessation of treatment);
- people who inject opioids;
- people who use prescription opioids, in particular those taking higher doses;
- people who use opioids in combination with other sedating substances;
- people who use opioids and have medical conditions such as HIV, liver or lung disease or suffer from depression;
- household members of people in possession of opioids (including prescription opioids).
People likely to witness an opioid overdose
- people at risk of an opioid overdose, their friends and families;
- people whose work brings them into contact with people who overdose (health-care workers, police, emergency service workers, people providing accommodation to people who use drugs, peer education and outreach workers).
Risk factors for overdoses with prescribed opioids include a history of substance use disorders, high prescribed dosage (over 100mg of morphine or equivalent daily), male gender, older age, multiple prescriptions including benzodiazepines, mental health conditions and lower socioeconomic status.
Emergency responses to opioid overdose
Death following opioid overdose is preventable if the person receives basic life support and the timely administration of the opioid antagonist naloxone. Naloxone, which is effectively an antidote to opioid overdose, will completely reverse the effects of an opioid overdose if administered in time. Naloxone is effective when delivered by intravenous, intramuscular, subcutaneous, and intranasal routes of administration. Naloxone has virtually no effect in people who have not taken opioids.
Access to naloxone is generally limited to health professionals. In many countries there is still limited availability of naloxone even in medical settings, including ambulances. At least one country, Italy, has already made naloxone available in pharmacies without prescription.
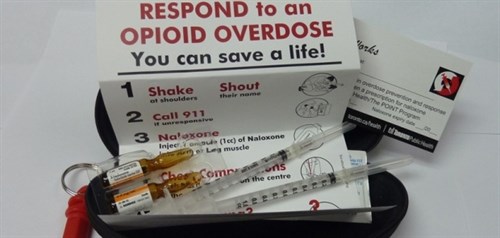
Since most overdoses are witnessed by a friend or family member, if a friend or family member had access to naloxone, he or she may be able to reverse the effects of opioid overdose, while waiting for medical care to arrive. While naloxone administered by bystanders is a potentially life-saving emergency interim response to opioid overdose, it should not be seen as a replacement for comprehensive medical care.
In recent years, a number of programmes around the world have shown that providing naloxone to people likely to witness an opioid overdose, in combination with training on the use of naloxone and on the resuscitation of people having an opioid overdose, could substantially reduce the deaths resulting from opioid overdose.
A recent survey in the United States found that the distribution of approximately 50 000 naloxone kits through local opioid overdose prevention programmes had resulted in more than 10 000 uses to reverse overdoses.
A number of countries and jurisdictions have started to adopt this approach. A policy of providing naloxone to people at risk of opioid overdose as well as to people likely to witness an opioid overdose has been in place in Scotland since 2011, and in a number of jurisdictions in the United States. Ireland has also announced this as a national policy. An evaluation of the impact of the policy in Scotland, which included people leaving prison as a target population, found that the proportion of opioid overdoses occurring within four weeks of leaving prison had halved since the introduction of naloxone.
Prevention of opioid overdose
Beyond approaches to reducing drug use in general in the community, specific measures to prevent opioid overdose include:
- increasing the availability of opioid dependence treatment, including for those dependent on prescription opioids;
- reducing irrational or inappropriate opioid prescribing;
- monitoring opioid prescribing and dispensing;
- limiting inappropriate over-the-counter sales of opioids.
The gap between recommendations and practice is significant. Only 42% of countries provide access to effective treatment options for opioid dependence and less than 10% of people worldwide in need of such treatment are receiving it.
WHO recommendations

- WHO recommends that naloxone be made available to people likely to witness an opioid overdose, as well as training in the management of opioid overdose.
- WHO recommends the use of a range of treatment options for opioid dependence which include psychosocial support, opioid maintenance treatments such as methadone and buprenorphine, supported detoxification and treatment with opioid antagonists such a naltrexone. WHO supports countries to introduce such treatment programmes where they do not exist.
- WHO supports countries in monitoring trends in drug use and related harm, to better understand when opioid dependence and opioid overdose is occurring. WHO supports countries to use medicines rationally, including medicines under international control such as strong opioids, to ensure the optimal of availability for medical purposes and minimization of their misuse and non-medical use.
- WHO recommends a stepped approach to the use of opioids in the management of cancer pain in adults – the WHO Cancer Pain Ladder, which recommends the initial use of non-opioids, then weak opioids, then strong opioids as pain increases. In the management of persisting pain in children, WHO recommends that weak opioids not be used, due to the variable metabolism of codeine in children. When prescribing opioids, WHO recommends measures to reduce the risk of misuse and diversion of opioids, including careful patient selection, and supervision of dosing where necessary.
Doctors can lead the way to healthier drug policies – join IDHDP now.
Share this on: